What constitutes familial ALS (fALS) and sporadic ALS (sALS)?
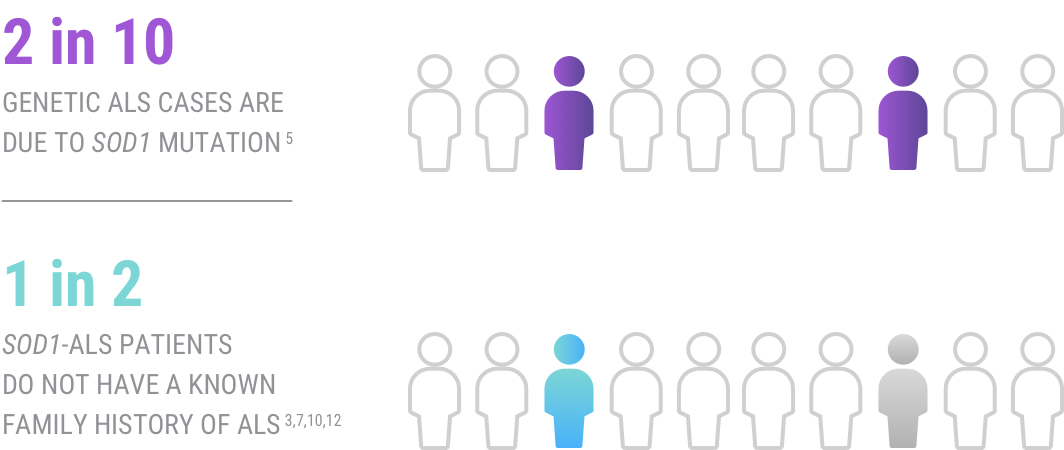
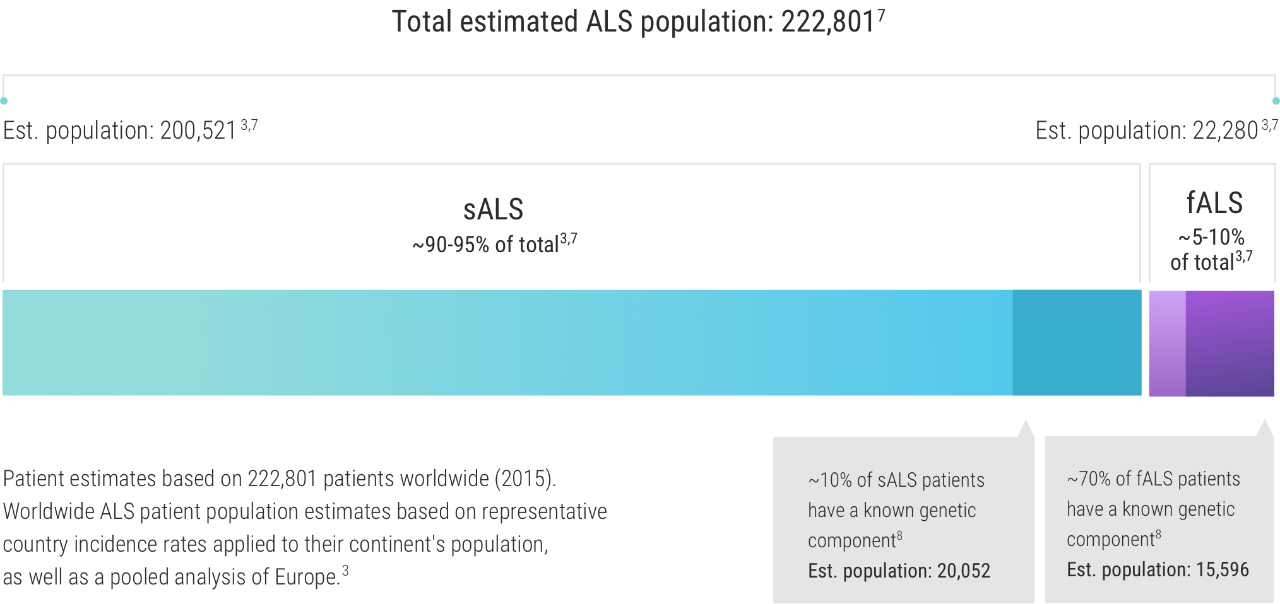
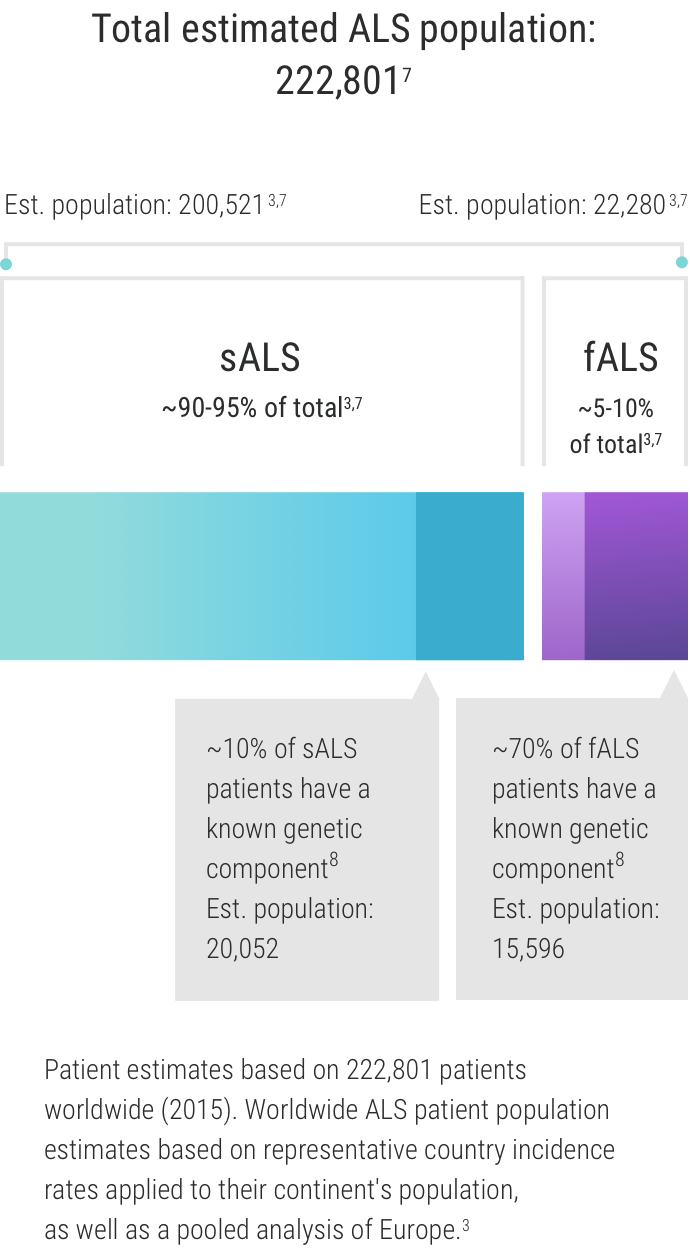
Approximately 5%-10% of all patients with ALS are thought to have fALS, while sALS accounts for about 90-95% of all ALS cases.1-3 There is now a deeper understanding of the role of genetics in ALS, which has provided new insights into the categorization of ALS. When referring to “genetic ALS”—we are not only referring to familial ALS. Recent discoveries showed that those diagnosed with both familial- and sporadic ALS have a genetic component to their disease. This has led to a deeper understanding of the disease—and new insights for researchers.3-6
There is no clear pathologic mechanism that can be ascribed to the development of ALS, but experts believe that an interaction among genetic, epigenetic, and environmental factors may play a role.5,9
While it may seem that a genetic association with ALS would only be found in patients with fALS since genetic mutations are inherited from one’s parents, this is not the case. This means that even if a patient has no known family history of ALS, a genetic component may still be involved.2